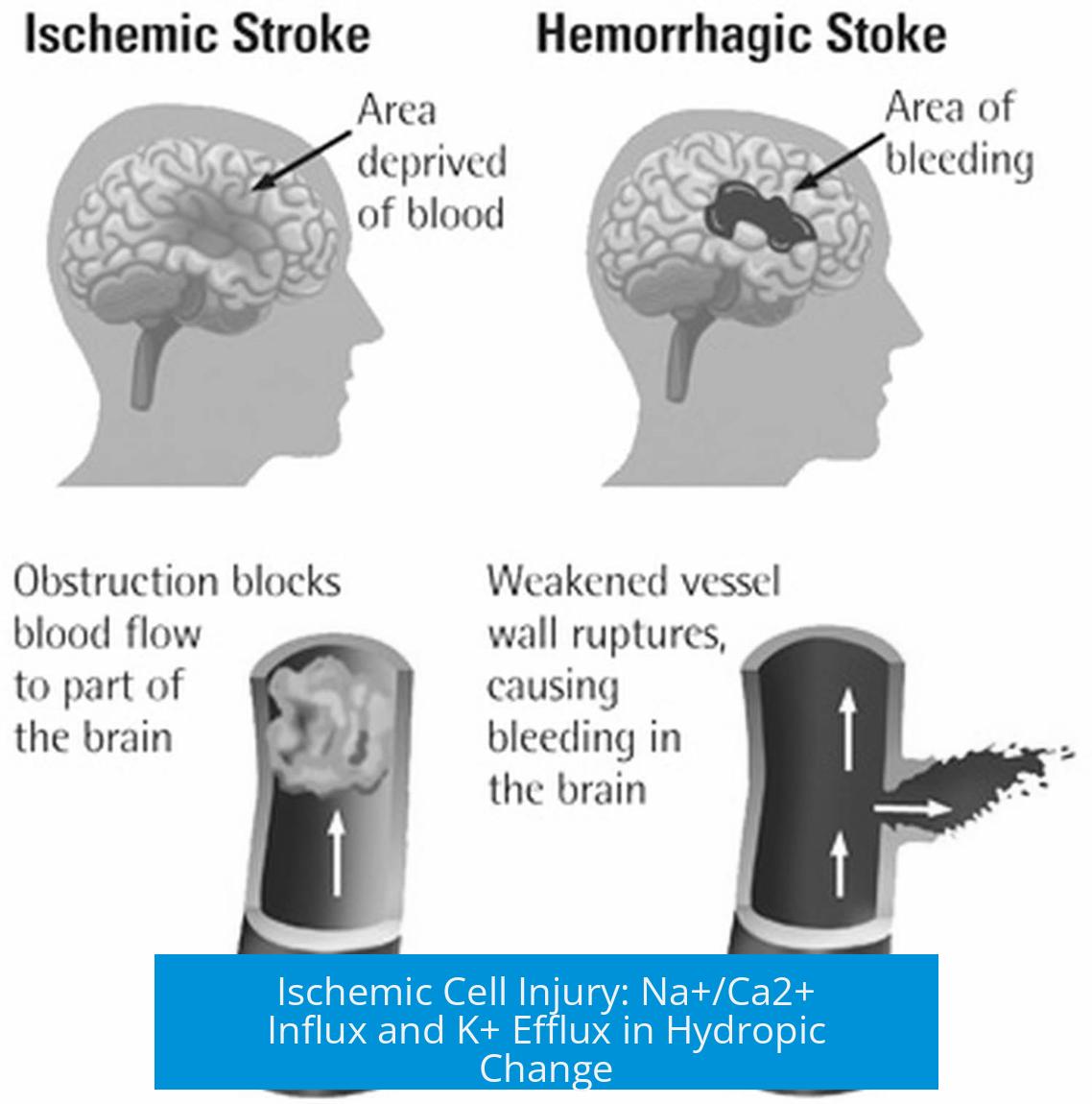
Ischemic Cell Injury and Hydropic Change: Role of Na+/Ca2+ Influx and K+ Efflux
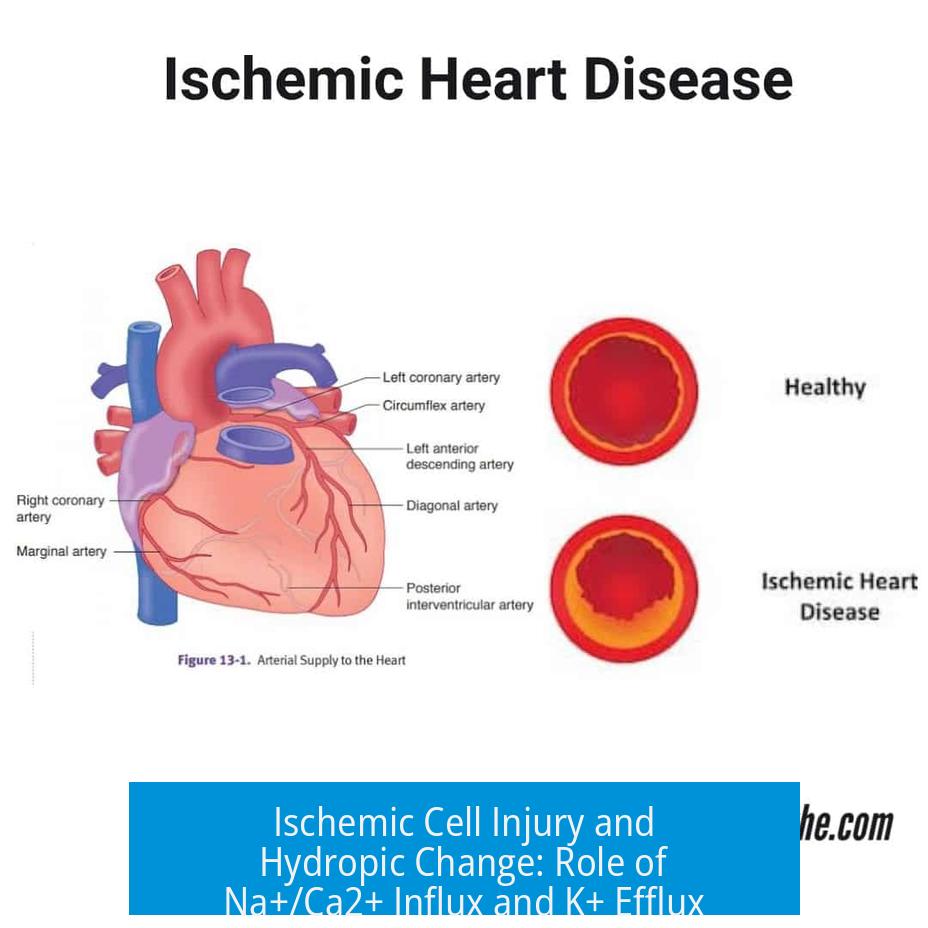
Ischemic cell injury causes hydropic change through a complex interplay of ion fluxes where ATP depletion impairs K+ efflux and volume-sensitive Cl− channels, while Na+ and Ca2+ influxes increase intracellular ion concentration, resulting in osmotic swelling despite attempts at ion regulation.
ATP Depletion Limits K+ Efflux
During ischemia, cells experience ATP shortage which compromises the ATP-dependent active transport of potassium ions (K+). Normally, K+ efflux helps maintain ionic balance and membrane potential. However, in ischemia, the cell’s reduced ability to pump K+ internally restricts its efflux.
This limitation means K+ cannot adequately exit the cell to counterbalance the influx of other ions.
Intracellular Na+ and Ca2+ Accumulate
Sodium (Na+) and calcium (Ca2+) ions increasingly enter the cell during ischemic injury. Elevated intracellular Ca2+ worsens injury by activating harmful enzymatic pathways. Simultaneously, elevated Na+ disrupts osmotic balance.
The buildup of these positive ions raises intracellular osmolarity, which promotes water influx and cell swelling—known as hydropic change.
Membrane Potential and Ion Gradients
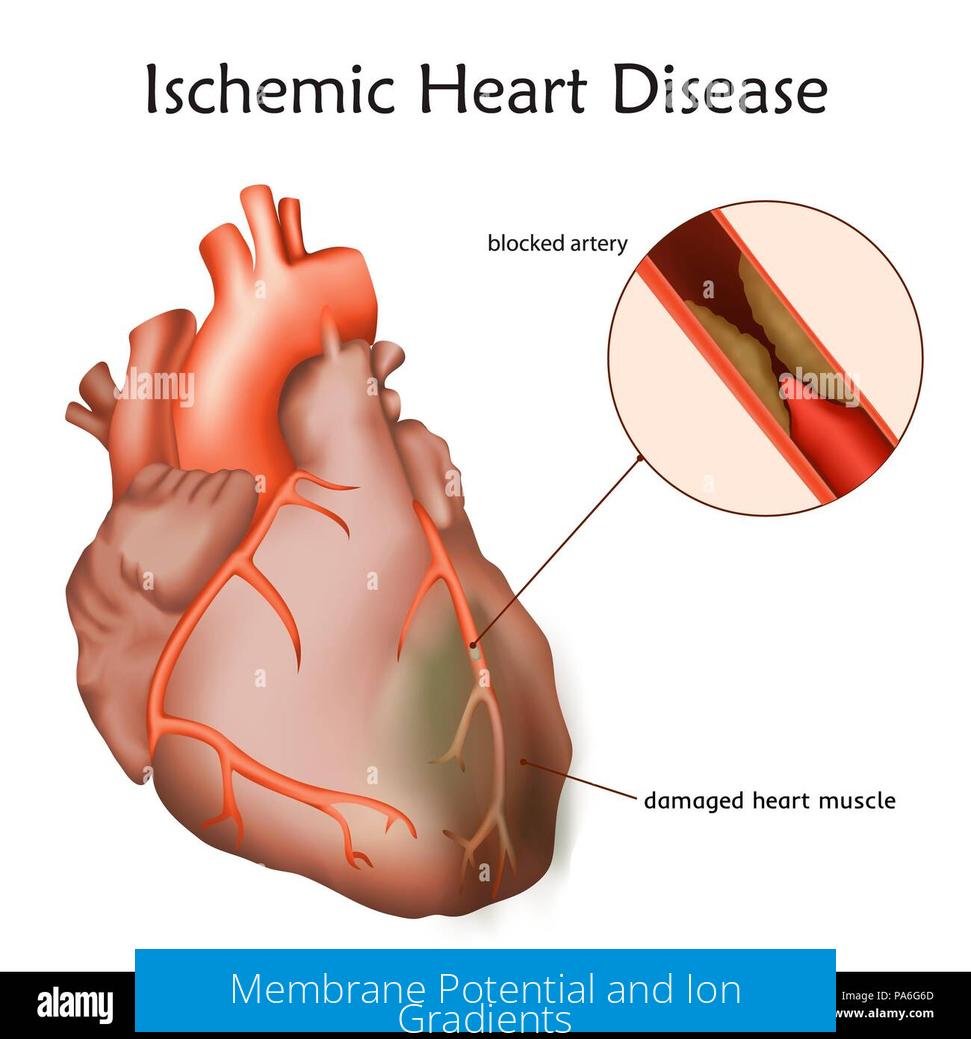
Membrane potential influences ion movement. Under ischemic conditions, altered ion gradients and membrane polarization occur. Although K+ typically moves out driven by concentration and electrical gradients, ischemia’s metabolic impairment limits this, reducing K+ efflux efficacy.
Why K+ Efflux Alone Cannot Prevent Swelling
K+ efflux initially may occur, transiently balancing osmotic pressure. But the net ion gain from Na+ and Ca2+ outweighs the loss of K+. Consequently, intracellular ion concentration rises, leading to increased osmotic pressure.
This imbalance causes water to enter the cell, driving hydropic swelling despite potassium loss. Experimental observations confirm early K+ efflux does not halt swelling progression.
Crucial Role of Chloride Ions and Their Channels
Chloride (Cl−) ions also regulate cell volume. Typically, cells respond to swelling by opening volume-sensitive K+ and Cl− channels to expel ions. Notably, Cl− channels are vital to reducing cell swelling.
Ischemia impairs these Cl− channels due to ATP depletion and lactic acidosis. Ion exchangers further raise intracellular Cl−, compounding ion accumulation. Loss of Cl− channel function removes an important protective mechanism against volume increase.
Summary of Ion Fluxes in Ischemic Hydropic Change
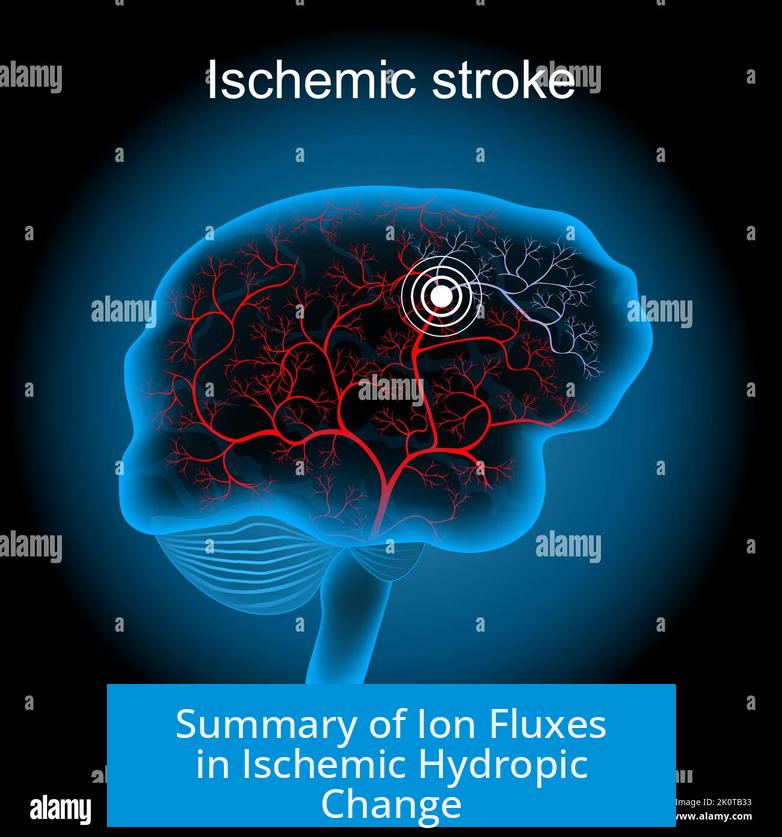
- Ischemia causes ATP depletion, impairing active K+ transport and Cl− channel function.
- K+ efflux is limited and insufficient to offset Na+ and Ca2+ influxes.
- Intracellular accumulation of Na+, Ca2+, K+, and Cl− raises osmotic pressure.
- Water influx follows, producing hydropic cell swelling.
- Cl− channel dysfunction exacerbates ionic imbalance and swelling.
Key Takeaways
- ATP-dependent K+ efflux and Cl− channel activity decrease in ischemia.
- Na+ and Ca2+ accumulate intracellularly, worsening ion imbalance.
- K+ efflux cannot prevent swelling due to net ion gain.
- Loss of volume-sensitive Cl− channels removes key volume regulation.
- Hydropic change results from osmotic water influx driven by ion accumulation.
Ischemic Cell Injury and Hydropic Change: How Na+, Ca2+, and K+ Ion Fluxes Stir the Pot
So, why does ischemia lead to hydropic change—or in simpler terms, cell swelling—and how do sodium (Na+), calcium (Ca2+), and potassium (K+) ions play starring roles in this drama? The short and punchy answer: ischemia depletes ATP, causing a breakdown in the cell’s finely tuned ion management system. This failure results in toxic accumulation of ions inside the cell, ultimately drawing water in and causing the cell to swell like an overstuffed balloon.
Got your interest? Let’s unpack this fascinating and critical process in lively detail.
The ATP Crisis: Why Ion Transport Stumbles in Ischemia
Imagine a busy city relying on electricity (ATP) to keep traffic lights (ion pumps) working smoothly. Now, if the power grid fails, chaos ensues. Similarly, ischemia starves cells of oxygen, crippling ATP production. This hits hard on the cell’s active transport mechanisms—especially the ATP-dependent pumps that shuttle ions across membranes.
One key victim is the Na+/K+-ATPase pump. Under normal conditions, it kicks three Na+ ions out and pulls two K+ ions in, maintaining the essential ion gradients that keep the cell’s volume and electrical balance stable.
Without ATP, this pump sputters and slows. Intracellular sodium rises as Na+ leaks in unchecked, and K+ builds up outside as its transport into the cell falters. But, why isn’t the cell simply ejecting K+ to compensate and prevent swelling? There’s a catch.
K+ Efflux: A Limited Lifeline
One might expect that cells would just yank out K+ to counter the swelling effect from Na+ influx. Well, cell membranes do allow some potassium efflux. Yet ischemic cells face two big hurdles:
- ATP Dependency: K+ transport relies on active processes, compromised due to depleted ATP.
- Efflux Limits: Cells can only lose so much K+ before internal functions falter. There’s an upper limit to how much K+ can safely leave.
Adding to the complexity, early in ischemia-induced necrosis, studies show an initial burst of K+ release—like a brief escape hatch. But this phase is temporary. Soon after, despite K+ attempting to leave, intracellular ion levels swell due to a dominant influx of Na+ and other ions. So, potassium efflux alone can’t keep the swelling monster at bay.
Calcium: The Silent Intruder
While Na+ plays the lead in swelling, calcium ions (Ca2+) sneak in and cause extra trouble. Normally kept at low intracellular levels, Ca2+ accumulates during ischemia because ATP-dependent pumps fail to expel it.
This calcium buildup triggers destructive enzymes and signals cell death pathways. It also worsens membrane damage and permeability, letting more ions flood in—creating a vicious cycle.
What About the Membrane Potential? Is It a Positive Inside Party?
You might wonder, “Does the cell’s electrical charge shift enough during ischemia to actually drive K+ out?”
Under normal conditions, the inside of a cell is negative compared to the outside, thanks largely to K+ gradients. But during ischemia:
- The membrane potential depolarizes—meaning it becomes less negative.
- This depolarization weakens the driving force for K+ to leave. Plus, with impaired pumps, maintaining gradients becomes impossible.
- Thus, the typical electrochemical push for K+ efflux diminishes.
The net effect? K+ efflux slows down just when the cell most needs to restore balance.
Chloride Channels: The Unsung Heroes That Quit Midway
Chloride ions (Cl-) join the ionic cast in swelling control. In healthy cells, K+ and Cl- channels open together to let ions flow out, shrinking the cell when needed.
But here’s the twist: volume-sensitive Cl- channels require ATP and a healthy pH to function. During ischemia, lactic acidosis (a drop in pH due to anaerobic metabolism) and ATP shortage knock out these channels.
Without working Cl- channels, the cell can’t rid itself of Cl- effectively. To make things worse, the Cl-/HCO3- exchangers increase intracellular Cl-, adding to the swelling pressure inside.
In short, losing chloride channel function is like taking away the cell’s emergency drain valve—water rushes in unchecked.
Hydropic Change: The Osmotic Consequence
So, the endgame? The combination of increased intracellular Na+, Ca2+, and Cl- ions raises osmotic pressure inside the cell. Water follows the ions by osmosis—the cell swells, sometimes painfully large enough to rupture membranes.
The “hydropic change” describes this pathological swelling—early signs of cell injury visible under a microscope as vacuoles form from excess water.
Bringing It Together – An Ionic Tug of War Losing Steam
Ischemic injury is a tale of balance upset and battle lost. Initially, cells attempt to field K+ efflux and maintain membrane potential, hoping to offset sodium influx. But ATP shortages, lost chloride channels, and rising calcium turn the tide against them. The net ion accumulation draws water in, causing hydropic change.
This detailed molecular chaos explains why simple ionic imbalances escalate into full-blown cellular damage. It also highlights therapeutic targets: can we protect or restore these ATP-dependent pumps? Could we stabilize ion channels under low energy states? Such questions drive ongoing research.
What Can We Learn and Apply?
- Clinicians: Recognize ischemic cell swelling as an early marker of injury severity. Interventions that restore energy supply quickly can halt the chain reaction.
- Researchers: Targeting volume-sensitive chloride channels may offer new protective strategies during ischemia.
- Students & Educators: Think of ion fluxes as the critical currency in cell survival—energy-poor states wreck the economy fast.
Next time you hear “ischemic cell injury,” picture a stressed cell gasping without ATP, with ions wildly crossing membranes, and water flooding the scene. Understanding how Na+, Ca2+, and K+ interplay paints an insightful story of cellular demise and survival.
Leave a Comment